And resistant strains will develop in a few months
I’m not a bacteriologist, but I do wonder why so much work is put towards finding new small molecule antibiotics instead of towards finding species-specific bacteriophages.
Both happen! It’s just work on phage therapy had to reinvent itself in the last decade or so and modern techniques are only just reaching maturity. We’re gonna see a lot more development in this space over the next decade.
I have not kept up on antibiotic resistance research, or phages in recent years.
I do recall a number of years ago, I believe in the US, someone scooping up pond and garden soil samples looking for new phages.
A quick search though, does show work on “phagemids”; the following article does mention that phages can cause harm to the human host by releasing harmful toxins in the bacteria when cell lysis is performed (potentially causing sepsis, or death), as well as bacteria do also develop resistance to phages over time.
https://news.mit.edu/2015/engineered-particles-kill-harmful-bacteria-0625
Don’t antibiotics also cause cell lysis? especially those like beta-lactams that interfere with cell wall maintenance
I think bacteriophages should be investigated much more, unfortunately I don’t think big pharma is that interested in them, although they are also pretty uninterested in antibiotics too, because they generally don’t make much profit. So I think at least in this economic model in the west we are unlikely to have them widely available. I am admittedly quite out of date, all I remember is that there was more research and use of them in eastern europe/russia.
They will, but there is also the chance that in gaining that new resistance, they may give up a different resistance, or become less lethal.
That’s the hopeful side of things; unfortunately, it is not uncommon for bacteria to develop resistance to a full combination of antibiotics over time, but I can be hopeful.
resistance genes are often carried on transferable elements like transposons and plasmids, which often contain multi-gene cassettes encoding for many types of resistance. I would also like to be hopeful too, but every antibiotic we have developed has had resistance develop against it, also within multidrug resistant strains like MRSA and CRAB. I think we should be hopeful for phage therapy, as well as AB + phage combination therapy. I think relying purely on antibiotics is a bit of a dead end.
🤖 I’m a bot that provides automatic summaries for articles:
Click here to see the summary
It does so with a never-before-seen method, cracking open an entirely new class of drugs that could yield more desperately needed new therapies for fighting drug-resistant infections.
The findings appeared this week in a pair of papers published in Nature, which lay out the extensive drug development work conducted by researchers at Harvard University and the Swiss-based pharmaceutical company Roche.
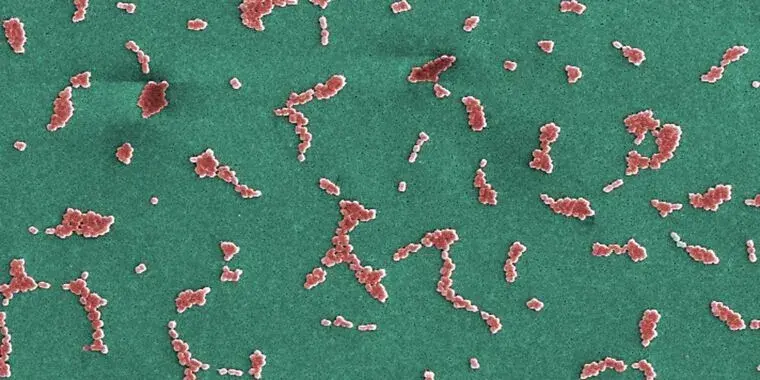
This category—which includes gut pathogens such as E. coli, Salmonella, Shigella, and the bacteria that cause chlamydia, the bubonic plague, gonorrhea, whooping cough, cholera, and typhoid, to name a few—is extraordinarily challenging to kill because it’s defined by having a complex membrane structure that blocks most drugs, and it’s good at accumulating other drug-resistance strategies
Though it may sound obscure, it’s an opportunistic, invasive bacteria that often strikes hospitalized and critically ill patients, causing deadly infections worldwide.
An international team of researchers, led by Michael Lobritz and Kenneth Bradley at Roche, first identified a precursor of zosurabalpin through an unusual screen.
But in this case, researchers searched through a collection of 45,000 bigger, heavier compounds, called tethered macrocyclic peptides (MCPs), which have weights around 800 daltons.
Saved 68% of original text.